
Establishing Molecular Diagnostics to Improve HIV Care and Management of Treatment Failure in Rural Lesotho

Making good diagnostics available in a rural resource-limited setting with an extremely high burden of HIV/AIDS
Know if your therapy works – The importance of viral load monitoring
In a person infected with HIV the virus replicates at an extremely high rate (more than 10 million virus particles can be found per milliliter of blood; thus a person can produce up to 50 billion new viruses per day). Yet, if this person starts taking antiretroviral therapy (ART) on a regular basis, virus replication can be completely blocked. If the medication works well in a person and if taken regularly, viral replication falls below the level of detection to <20 viruses/mL. This status is called "undetectable" or "virally suppressed". This achievement results in two major benefits:
- A person with continuously suppressed HIV is much less likely to develop AIDS or to die from HIV;
- A person with suppressed HIV through ART is very unlikely to transmit the virus to others.
However, a person may fail to achieve HIV suppression while taking ART – either because he/she does not take the medicine regularly, or because HIV has become resistant against one or several of the drugs in the treatment regimen. Failure to suppress HIV can only be diagnosed reliably through a "viral load measurement", which determines the number of virus particles in the blood. When treatment failure has been diagnosed, the care-provider can intervene by supporting the patient to take the drugs regularly or by changing the drugs of a treatment to those, for which the virus is not resistant.
Antiretroviral therapy with no viral monitoring – blind flying in Sub Saharan Africa
Unfortunately, measuring viral loads is cost-intensive, requires dedicated laboratory equipment and highly skilled technicians. As a result, even though recommended by the World Health Organization, most HIV infected persons taking ART in resource-limited settings do not receive any viral load measurement. The large majority of the over 12 million patients taking ART in Sub-Saharan Africa receive therapy without a reliable control if this treatment works. They might therefore uselessly continue taking their drugs despite a high viral load with resistant virus, and their health care provider may not even be aware of it. As such these patients can – although they are under therapy – develop AIDS and die, and they can transmit HIV to their sexual partners.
Regular viral load measurement is therefore absolutely key for good-quality care for persons living with HIV!
Making viral load monitoring now available in Butha-Buthe, Lesotho
Lesotho, a small land-locked country surrounded by South Africa, has the second-highest HIV-rate in the world with one out of four adults being infected with HIV. The "Towards 90-90-90 Consortium" has joined forces to make viral load monitoring accessible to all patients receiving ART in the district of Butha-Buthe in Northern Lesotho. A dedicated laboratory has been set up end of 2015 and was inaugurated by the Honourable Minister of Health, Dr. 'Molotsi Monyamane on June 16, 2016. With this Butha-Buthe became the first district in Lesotho where all patients on ART have access to regular routine viral load monitoring.
 The Honourable Minister of Health, Dr. 'Molotsi Monyamane, officially inaugurates the Molecular Laboratory in Butha-Buthe on June 16, 2016
The Honourable Minister of Health, Dr. 'Molotsi Monyamane, officially inaugurates the Molecular Laboratory in Butha-Buthe on June 16, 2016
 The fully-automated viral load platform in Butha-Buthe Laboratory
The fully-automated viral load platform in Butha-Buthe Laboratory
A high viral load must lead to action! -- the Viral Load Monitoring Database
Measuring the viral load in blood can only be beneficial to the patient if the health care provider takes appropriate measures to achieve viral (re-)suppression when the viral load value was high: The health care provider must assist the patient in improving his/her adherence (taking the pills regularly) and, whenever despite good adherence the viral load remains high, the patient must be switched on a so-called second-line therapy. Such a second-line therapy consists of drugs different from first line in order to overcome accumulated resistances of HIV.
To ensure that not a single one of the many patients, who receive viral load monitoring in Butha-Buthe gets missed, we have now set up a confidential and secured new database, which allows those persons, who are directly involved in patient management, to identify all patients, who have unsuppressed viral loads. This shall ensure that these patients, who are immediately threatened to progress to AIDS and who are at highest risk to transmit HIV to others despite therapy, get the care they need for achieving resuppression as soon as possible.
The link below leads to an aggregated and anonymized report on the viral loads conducted during the last six months. The report is real-time updated every time a new viral load result is confirmed in the database.
More detailed report: https://lstowards909090.org/db/publicstats/report5
Know why your therapy doesn't work – Genotyping in rural Lesotho
In countries with sufficient financial resources viral load monitoring and resistance testing have become a clinical "must". In many rural African settings, however, none of these have been implemented as solid routine services until today.
With the successful establishment of viral load monitoring in Butha-Buthe district, our consortium has now begun to set up genotypic resistance testing for HIV, because in persons with persistently unsuppressed viral load it will now be key to understand why they fail to achieve viral suppression. Genotypic resistance testing helps to see if any and what kind of resistance HIV has developed in a given patient. This information will then allow the physician choosing a best alternative treatment option.
End of September 2016 the laboratory team in Butha-Buthe district successfully generated for the first time in Lesotho HIV resistance profiles for clinical use.
 State-of-the-art processing of more than 250 viral load samples every week at the laboratory in Butha-Buthe
State-of-the-art processing of more than 250 viral load samples every week at the laboratory in Butha-Buthe
The project of genotypic resistance testing has two long-term goals:
- To improve the individual patient management and to guide optimal drug choice for patients with treatment failure
- To build in Lesotho the capacity for nationally conducting resistance testing with the possibility for health care providers and laboratory technicians from and in Lesotho to broaden their professional skills and to conduct competitive research relevant to the field.
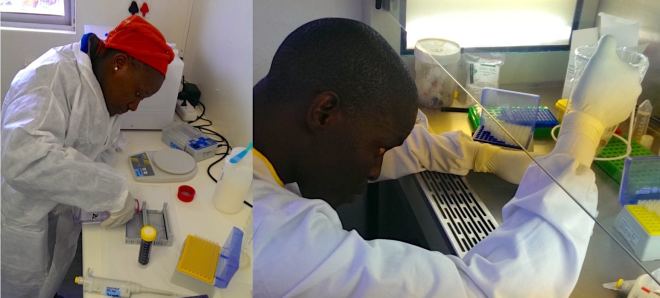 Preparing samples for genotypic sequencing
Preparing samples for genotypic sequencing
 The 27th of September 2016: The first genotype ever conducted successfully in Lesotho. The proud team stands in front of the computer displaying the genotypic results from the first patient sample
The 27th of September 2016: The first genotype ever conducted successfully in Lesotho. The proud team stands in front of the computer displaying the genotypic results from the first patient sample
The Towards 90-90-90 Consortium
Swiss Tropical and Public Health Institute (www.swisstph.ch)
- Contacts: Niklaus Labhardt (Project Leader; n.labhardt(at)unibas.ch); Tracy Glass (Project Leader) (tracy.glass(at)unibas.ch)
Molecular Virology, Department of Biomedicine, University of Basel (https://biomedizin.unibas.ch/home/)
- Contact: Thomas Klimkait (Head of Research Group; Thomas.klimkait(at)unibas.ch)
SolidarMed, Swiss Organization for Health in Africa (www.solidarmed.ch)
- Contact: Josephine Muhairwe (country coordinator Lesotho; j.muhairwe(at)solidarmed.ch); Christiane Fritz (desk-officer; c.fritz(at)solidarmed.ch)
Research Coordination Unit, Ministry of Health of Lesotho
- Contact: Kyaw Thin (Head of Unit; dr.kyawthin(at)gmail.com)
District Health Management Team of Butha-Buthe
- Contact: Lebohang Sao (District Health Manager)
Central Laboratory Services of Lesotho (Ministry of Health)
- Contact: Tsietso Mots'oane (Head of Unit)
Laboratory Services of Seboche Hospital
- Contact: Molisana Cheleboi (Head of Laboratory; mcheleboi(at)gmail.com)
Funding
This project receives partial funding by:
- r4d programme (www.r4d.ch), a joint funding initiative by the Swiss Agency for Development and Cooperation and the Swiss National Science Foundation
- ESTHER Switzerland who is supported by the Swiss Agency for Development and Cooperation
- Gottfried Bangerter-Rhyner Foundation
However, to expand and sustain access to molecular diagnostics for persons living with HIV, additional funding for further strengthening of the laboratory is needed.